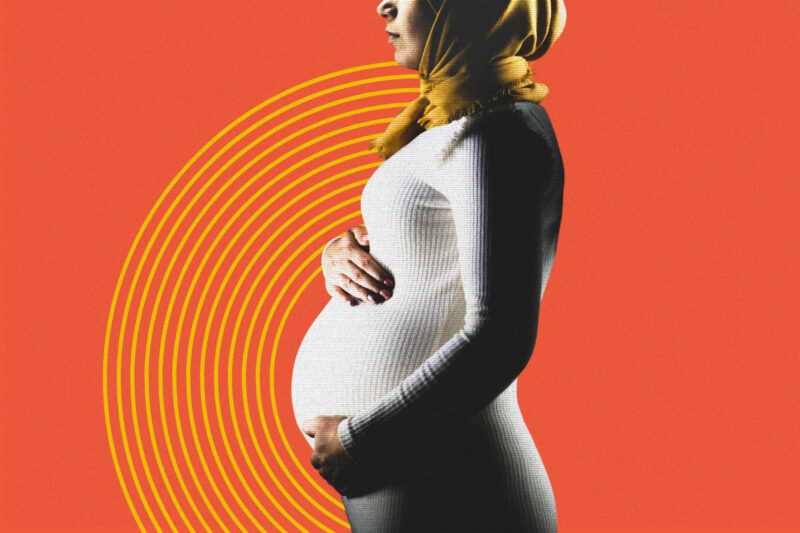
South Asian women with postnatal depression benefit from culturally adapted therapy, study finds
Research suggests therapists who speak patients’ language and understand mental health stigmas can speed recovery

South Asian women with postnatal depression may be 40% more likely to recover quickly if they receive therapy that is tailored to their cultural needs instead of the usual treatment provided by a GP, new research suggests.
One barrier the researchers sought to overcome was the problem of therapists and doctors with limited knowledge of South Asian communities failing to understand stigmas about mental health, resulting in services that are inaccessible or ineffective for some. Another was the problem of isolation, with therapy instead delivered at group sessions with a creche.
The study, published recently in The Lancet, screened more than 4,000 South Asian women from across the UK and found that those who took part in culturally sensitive therapy for 12 weeks were more likely to recover from postnatal depression within four months than those who didn’t.
While British South Asian people are marginally more likely to experience mental health issues than white people, they are around 30% less likely to contact mental health services. Additionally, Asian women are twice as likely to experience health complications during and after pregnancy compared with white women.
Nusrat Husain, professor of psychiatry at Manchester University, who led the study, said the findings showed that South Asian women “are not hard to reach”.
“We have shown that South Asian women would love to engage with mental health services, but we need to develop trust within these communities,” Husain said.
“Many of them have felt excluded, or may have been burnt before where their experience with the NHS has not been great. But if we work with an approach that has cultural humility as its focus, we can engage them.”
The study was carried out in towns and cities across the UK, including Manchester, Bolton, Rochdale, Oldham, London, Nottingham, Leicester and Glasgow.
Researchers recruited women for the study by working with local community centres as well as gurdwaras, temples and mosques. Some mosques promoted the project at the end of sermons and encouraged families to take part.
After initial screening, a total of 732 women were selected to participate in the trial — 88% of whom were Muslim. Of these women, half of the cohort took part in a course of 12 group sessions of culturally adapted therapy, while the control group had the treatment usually offered by a GP.
This standard treatment for postnatal depression includes encouraging self-help, such as talking about your feelings with friends and family, regular exercise and eating a healthy diet. Women may also be referred to a course of talking therapy, or prescribed antidepressants.
Under the culturally adapted talking therapy, women were invited to therapy sessions delivered in Urdu, Punjabi, Tamil, Gujarati and Bengali as well as English.
The sessions focused on the challenges of being a British South Asian woman, the role of religion and spirituality in mental health, issues affecting self-esteem, exercise, relaxation, assertiveness, self-confidence and tackling social isolation.
The study found that 56% of women who had culturally adapted therapy had recovered from postnatal depression after four months, compared with 40% of women from the control group.
Amina Hatia, co-midwifery manager at Tommy’s, a pregnancy and baby loss charity, described good maternal mental healthcare as a “postcode lottery” for the general population.
“Sadly postnatal care and maternal mental health care have been chronically underfunded,” she said. “When it comes to things like maternal mental health care, there’s almost this idea that it’s a ‘nice to have’ rather than an absolute necessity.”
Hatia said the situation was only made worse for South Asian women due to the additional barriers they face. One such barrier is that health professionals often assume South Asian women need less support because they come from a community with a tradition of strong family ties.
“Healthcare professionals don’t probe around depression and how the mother is feeling because they assume they have support, as opposed to someone who presents as isolated,” Hatia said.
“They think that because you’ve got your family, you have people to look after you, without taking into account that women don’t always have someone to talk to or the close relationships they are assumed to have.”
Practitioners who helped deliver the culturally adapted therapy said some of the adjustments aimed to address the stigma around mental health disorders in South Asian communities.
This included limiting the use of terms such as depression and anxiety when talking to the women about how they felt, and instead using words like low mood, sadness, and worry. There was also the availability of a free creche, where women could leave their children while they attended the sessions.
Afsana Tutla, a psychological wellbeing practitioner for the NHS in Blackburn, said this was vital in ensuring women attended therapy sessions. “It meant that many of them could tell their family they are going to a children’s group, and wouldn’t necessarily have to say they were going to counselling.”
The therapy was also delivered in group sessions. “A lot of women felt very alone, like whatever they were going through was only happening to them. But actually, coming together allowed them to share their experiences and realise they could understand and support each other,” Tutla said, adding that many of the women formed friendships and still keep in touch.
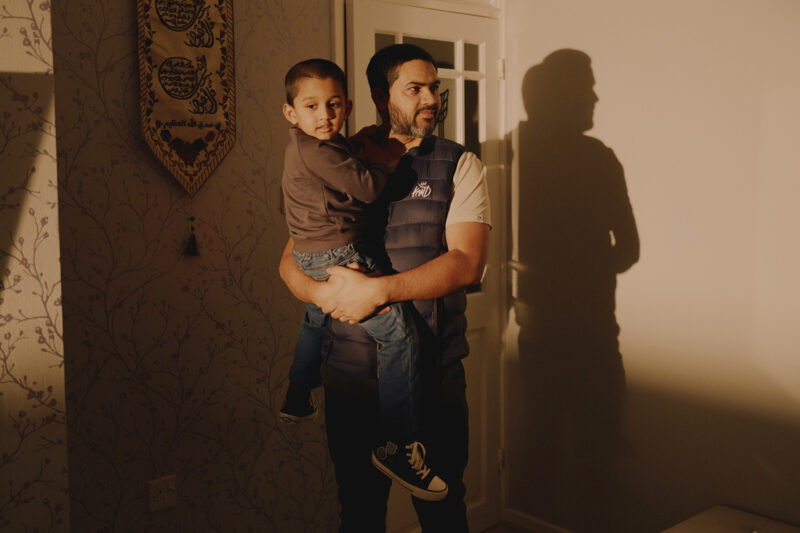
Following the 12 sessions of therapy, researchers carried out assessments of the women’s mental health, often at their family homes.
They found that women responded best when the health visitor could speak their mother tongue or had a similar cultural background.
This ensured that if the mother wasn’t fluent in English, another family member didn’t need to act as a translator. “This meant we could speak to the woman on her own, because we found they wouldn’t truly open up about how they feel if other people were present,” Tutla said.
“But even if the mother was fluent in English, we found that having someone who understood the culture made the home visit more comfortable.”
In the UK, registered charity Maternal Mental Health Alliance has a network of more than 130 organisations who provide mental health support, information and advice for mums and families during pregnancy and after giving birth.
 Newsletter
Newsletter