‘Women struggling with fertility tend to feel isolated’
Biological treatments like IVF often come with a host of moral and religious dilemmas
–
Five years into her marriage, Sara Khan, then 30, still was not pregnant and starting to despair. She and her husband are from a close-knit British-Pakistani community in Manchester, and had grown up with the assumption that life would follow a certain path: go to university, get a job, get married, have children.
So it was a shock when childbirth suddenly seemed out of reach. After five years of privately dealing with the grief of infertility — the unwanted period each month, painful questions from well-meaning relatives — the couple sought advice from their GP. Sara and her husband, who are both practicing Muslims, discussed the medical advice; they’d been recommended IVF. Khan’s husband’s first instinct was that if God’s plan was for them to have children, then he would provide them. Khan’s view was that it was God who had allowed humans to develop the scientific knowledge to assist in reproduction in the first place.
“I really couldn’t see a theological reason not to do it,” she told me. “And the thought of not doing it just felt unbearable. I had to know that I had tried everything.” They decided to proceed with IVF.
More than 50,000 people in the UK have IVF every year with some — like the Khans — receiving treatment through the NHS, but the majority having to pay privately. Costs range from £3,000 to £5,000 for a standard cycle of IVF, but can be up to £20,000. NHS treatment is typically limited to three cycles per couple — if it’s available. Access to IVF is a postcode lottery. Someone in Scotland, for instance, can typically access more funded cycles than someone in London. Waiting times also vary hugely in different areas, all of which pushes people into private care which can cost tens of thousands of pounds, making it prohibitively expensive for some.
Infertility is a painful, isolating and stressful experience for anyone. For Muslims, this can be compounded by a prevailing cultural pressure to have children and stigma around discussing infertility and pregnancy loss. Muslim women can also mistrust the NHS, which has repeatedly been shown to have worse outcomes for women of colour. Last year, an inquiry into racial injustice in maternity services by British charity Birthrights found that Black, brown and minority ethnic women were often ignored, dismissed, subject to coercion from caregivers and disproportionately affected by structural barriers to care. Other studies have found that British Bangladeshi and Pakistani women are significantly less likely to receive pain relief in birth than white women, by 24% and 15% respectively.
While having a family is not a religious requirement in Islam, religious texts emphasise the importance of the institution of marriage and the family structure. “There’s a huge, undeniable emphasis in Islam to have children,” said Dr Mona Elgohail, a US-based clinical psychologist who has studied Muslim women’s experiences of infertility. “Muslim social life is often very centred around families. Women struggling with fertility tend to feel isolated, and to get a lot of comments — like ‘have you thought about having kids?’”
Religious beliefs also profoundly shape the way that Muslim women experience infertility; sometimes it can provide a huge comfort, but for others the prolonged struggle to have children can lead to a loss of faith. There can also be — as Khan and her husband experienced — conflict over how theology should inform practical decisions over fertility treatment.
A Muslim GP based on west London, who asked not be named because her parents don’t know about the extent of her pregnancy loss, said she has noticed that women of Muslim backgrounds often seek medical support later than might be expected. She suspects this is due to cultural stigma around speaking up about infertility and being unaware of when to get help.
“The thing I have found most challenging with Muslim women is that many come in not having spoken to their husband, whereas white British couples may come in together,” she said. “I have to say ‘please, please bring your husband in’, because I can’t make a referral to a fertility clinic until both partners have been tested. I think this is changing generationally, gradually, but it’s still an issue.”
Faith itself can also play a role in how women cope with infertility, as the doctor discovered herself. She conceived her first child easily, but had six miscarriages while trying for a second. “I’m a doctor, I know the stats about how many pregnancies end in miscarriage, but that doesn’t prepare you for the hope of each pregnancy test,” she said. “You can’t put it into words, that lack of control.”
She told her parents about the first two losses. “After that, I just spoke to my Lord. I literally just prayed, crying: ‘OK, this has happened, I leave it to you, it goes to you in heaven, it’s your choice, your decision’.”
She and her husband turned to religion — they drank holy water from Mecca, donated regularly to charity and prayed for forgiveness from their sins. Eventually, she reached a kind of peace. “Getting there was very, very hard. I’m a medic, and we don’t give up easy, we work hard. But getting to the stage of submission — a complete submission to his plan — was when I found peace.”
After many months of struggling, she had a healthy second pregnancy and became pregnant with her third child without trying. “It just goes to show, God is the greatest planner of all,” she said.
Faith was a comfort to her, but this is not the case for all women. In 2016, Elgohail launched a study, the Muslim Fertility Project. The study took the form of an online survey assessing stress and depression levels among Muslim women with infertility who were living in Australia, Canada, the US and the UK.
Elgohail initially anticipated a problem in getting enough respondents. However, the Facebook video announcing the project has now been viewed more than 200,000 times — not a typical outcome for a call-out for participants in a psychological survey.
“We were floored by how many people responded,” she said. “It seemed like it shattered a wall of silence, and showed that this understudied group of women are ready to share, and to ask for help.”
The final study included almost 500 women trying to conceive, and found high levels of stress and depression. It also found that women were using religion both positively — like the west London doctor — and negatively, which included feeling abandoned or punished by God, a religious thought pattern often associated with depression.
Elgohail also found her Facebook Messenger inbox flooded with messages from men and women sharing their own painful stories and asking for advice. Seven years after launching her study, Elgohail still regularly receives questions, and has compiled a list of religious scholars to share with those who seek help.
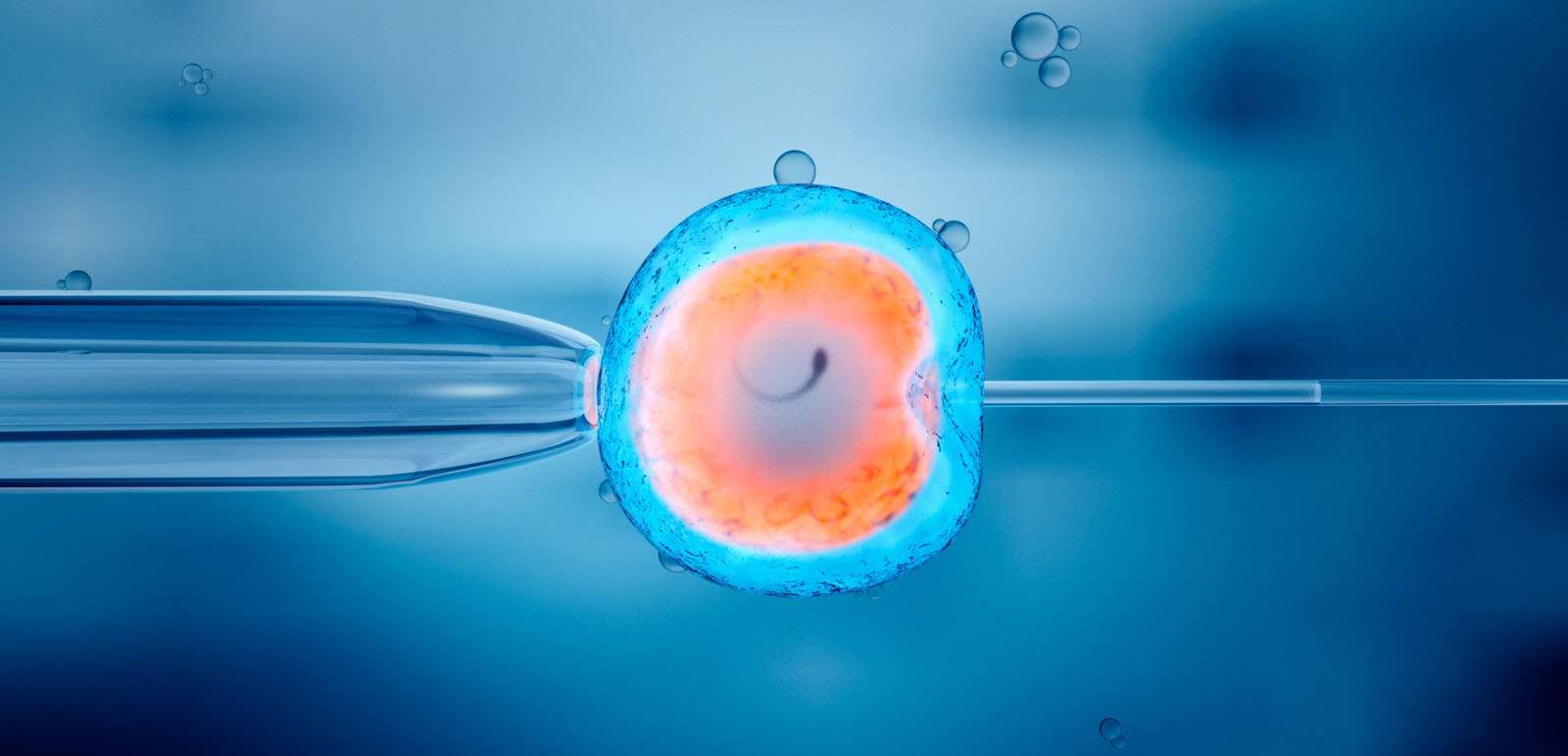
Artificial reproductive technologies such as artificial insemination and IVF are relatively recent developments and are obviously not mentioned in Islam’s primary texts. Yet most contemporary religious scholars and institutions, including the Islamic Fiqh Council in Mecca agree that assisted reproduction is permitted in Islam, as long as it uses the husband’s semen and the wife’s egg and womb — meaning that donor eggs or sperm and surrogacy are prohibited.
These religious boundaries can lead some couples to seek out scholars espousing the minority opinion that third-party donation is allowed — there are some clinics in Iran that allow the use of donor eggs or sperm, following a 1999 fatwa by Ayatollah Khamanei. Elgohail has also received letters questioning what to do with unused embryos. “That might be questions such as, what is their status religiously? Can they be discarded, or donated? These women carry some guilt, fear and anxiety around not doing the right thing.”
Sara Khan and her husband found themselves with precisely this conundrum when they began their treatment six years ago. Several rounds of IVF produced a number of healthy embryos, and they eventually had two children — but they still had a number of frozen embryos. “We didn’t know what to do with the embryos, religiously. The options were to destroy them, which felt wrong, or to donate them for science,” said Khan.
The imams at their local mosque were equally unsure and much of the advice they found online was contradictory. Some scholars said each embryo is a human life and it was therefore unacceptable to donate any for scientific research, others argued any embryo did not count as a life while it existed outside the womb.
“It left our heads spinning,” said Khan. For the past six years, the couple has opted to use an NHS service which allows couples to keep embryos for up to 10 years for an annual storage fee of £127.
“We keep putting the decision off while we try to assess the correct thing to do,” said Khan. “Maybe in the end it’ll be the NHS that decides for us — would that still be God’s will?”
Topics
Get the Hyphen weekly
Subscribe to Hyphen’s weekly round-up for insightful reportage, commentary and the latest arts and lifestyle coverage, from across the UK and Europe
This form may not be visible due to adblockers, or JavaScript not being enabled.