‘In some cultures menopause is not even spoken about’
From social stigma to a lack of culturally appropriate care, a variety of overlapping factors are impeding access to treatment for minority ethnic patients

When Juwairiyyah Abubakar was 40 years old, a routine doctor’s appointment confirmed she was going through the menopause. The diagnosis made the hot flushes, sweating and mood swings make sense. Although she grew up in Nigeria where menopause wasn’t discussed among women, she knew from friends and her own research what to expect during the process.
Since then, Abubakar, now 43, has been managing her symptoms on her own. She has not sought medical treatment, preferring to go through the process as naturally as possible.
“I had a friend who was prescribed HRT (hormone replacement therapy) to manage her symptoms and it caused her some health issues,” says Abubakar. “After seeing her experience, I knew I didn’t want medication. I don’t want to put anything new in my body when I could just be patient and wait it out.”
HRT is a common treatment for managing menopause and perimenopause — the period preceding menopause when levels of oestrogen in the body rise and fall unevenly. In November, the health assessment body Nice updated its menopause guidelines for medics in England and Wales, stating that HRT should be offered as a first-line treatment.
However, disparities in access to menopause-related care and treatment among Black, Asian and minority ethnic women exist. The Fawcett Society’s 2022 report Menopause and the Workplace highlighted the gaps in access to menopause care, with 45% of Black and minority ethnic women surveyed experiencing delays in diagnosis, compared to an overall average of 31% of women.
According to a recent study presented at the World Congress on Menopause in Melbourne in October, women of Black, Asian and minority ethnic backgrounds are around 80% less likely to receive HRT treatment, which is commonly administered in the form of patches that are applied to the skin and release hormones into the body. The 10-year study by academics at the University of Oxford examined the HRT prescriptions issued in England to almost two million women aged between 40 and 60.
Findings revealed that Chinese women were 82% less likely to receive HRT, while Black African women were 79% less likely. Pakistani, Bangladeshi and Indian women were 70%, 64% and 61% less likely to be receiving HRT, respectively. Alongside ethnicity, the study also factored in age and deprivation, with women in the most deprived areas even less likely to take up HRT, compared to their white peers and those in more affluent areas.
But there are many additional factors to consider. According to Dr Aziza Sesay, a GP based in the West Midlands, cultural competence in healthcare, poor health literacy and limited access to care, all play a role in the disparities in access to HRT.
“In some cultures, menopause is not even really spoken about as it is a taboo and stigmatised topic,” she says. “It’s usually seen as something to be managed without medication so women steer clear of it and opt for more lifestyle-based or natural remedies.”
Sesay adds that there is also a need for the NHS to involve more grassroots organisations in order to raise awareness about menopause and HRT. She runs an online platform called Talks with Dr Sesay, sharing information on a range of topics, in particular, women’s health, cancer awareness and health equity.
“Some people do not believe that they can experience menopause because they don’t see themselves represented in public campaigns. It often tends to showcase older, affluent white women,” she adds.
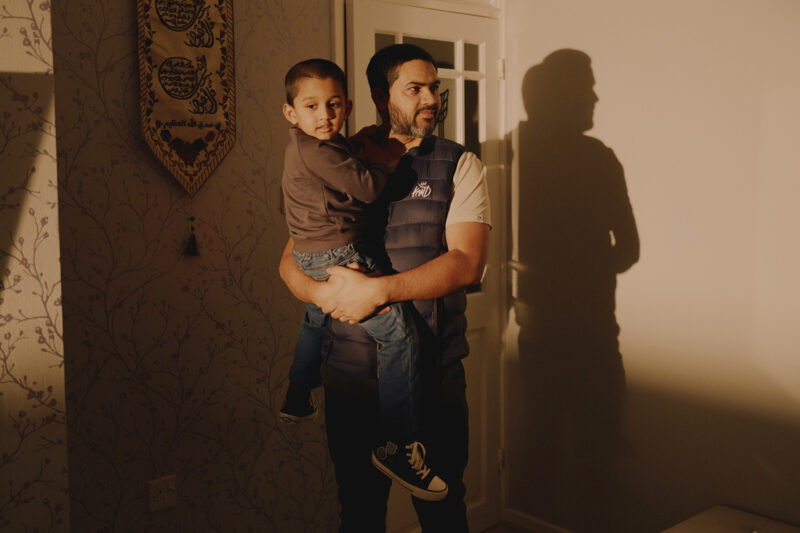
Shakeelah Perviaz, 52, is also cautious about taking HRT after seeing the effect on other women she knows. The mother of eight children learned she was perimenopausal during a routine medical check-up related to her diabetes. Over the past seven years, she has experienced various symptoms, including tiredness, hair loss, aching joints and mood swings.
“Some of the stories I’ve heard — that you have to be on it for life and there’s a high risk of cancer and more — have scared me,” Perviaz says. “So far I’ve taken care of myself, but if it gets to a point where I’m not coping, then maybe I’ll consider getting a mild dosage of patches.”
Many women are concerned that HRT increases the risk of conditions such as breast cancer and heart disease. However, according to NHS guidance, extensive research has shown that for most women, it is a safe and effective treatment and the adverse effects are minimal. Furthermore, the additional benefits of HRT, including the maintenance of muscle strength and the prevention of osteoporosis, far outweigh those small risks for many women.
Raj Johal, 44, is the founder of South Asian Menopause Support (Sams), an online platform where she provides one-to-one menopause support to women. In her experience, a significant number of Muslim women are hesitant to talk about their menopause experience due to stigma, further excluding them from access to treatment.
Johal has been using HRT patches for the past two years and says that her symptoms have become more manageable. However, she has found that a deep-rooted fear of the side effects caused by HRT remains among many women of South Asian heritage.
“There’s an assumption that HRT causes breast cancer or can lead to other health issues,” says Johal. “It’s also to do with your private parts and women’s health, which are just not things we discuss in the South Asian community. These are just some of the taboos caused by the older generation. They probably didn’t know what they were going through and also didn’t get the necessary support.”
The challenges in accessing treatment don’t stop with cultural stigma. According to Johal, sometimes language barriers and age-related biases — Black and Asian women tend to go through menopause earlier than their white peers — play a part.
The lack of effective communication between patients and medical professionals is also an important factor. Sometimes, the women themselves do not understand what they’re going through, which further complicates the doctor’s ability to interpret their symptoms, Johal adds.
“It’s a double-edged sword,” she explains. “Many of these women don’t open up fully to their doctor about everything they’re going through. On the other hand, doctors are often short on time and can’t delve deeply. As a result, they may do the bare minimum and dismiss symptoms by saying, ‘You’re too young for HRT’. It takes a doctor with both the time and determination to get to the root of the problem.”
For Johal, the experiences of women such as Abubakar and Perviaz highlight the need for a more inclusive and culturally sensitive approach to menopause care. While platforms such as Sams exist, there is still a long way to go to break down the cultural taboos and encourage more open conversations within communities, says Johal.
“We need more menopause champions in the community. We need more focus groups and clinics addressing our needs and concerns,” she says. “A lot of women have nowhere to go.”
 Newsletter
Newsletter